Pelvic organ prolapse Whererei
A pelvic organ prolapse happens when the tissues and muscle that support your pelvic organs become weak. This can cause one of your organs to drop down and bulge into your vagina.
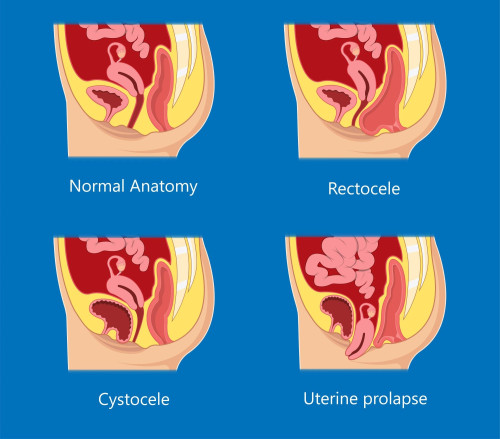
Types of pelvic organ prolapse
There are different kinds of prolapse, depending on which organ has dropped. These include:
- uterus (uterine prolapse)
- bladder (cystocele)
- rectum (rectocele).
Causes of a pelvic organ prolapse
Anything that weakens or stretches your pelvic floor muscles and ligaments can increase your risk of getting a prolapse. This includes:
- pregnancy and childbirth, due to the weight of your pēpi, hormone changes, labour and childbirth
- often straining to do poos
- being an unhealthy weight
- repetitive heavy lifting
- regular coughing or sneezing such as from smoking, asthma or hay fever
- ageing, which causes loss of muscle tone
- menopause, which lowers levels of estrogen and makes your muscles less elastic
- previous pelvic surgery, which may have damaged nerves and tissues in your pelvic area.
Symptoms of a pelvic organ prolapse
Depending on which organ has prolapsed, you could experience:
- a feeling of heaviness or pressure in your lower belly
- a feeling of a bulge or something coming down or out of your vagina
- discomfort during sex
- difficulty doing poos
- wee (urine) leaking when you cough, sneeze or exercise (known as stress incontinence)
- problems when you wee, such as the wee coming in a slow stream or a feeling of not fully emptying your bladder.
Sometimes there are no symptoms. The prolapse may only be discovered during a pelvic examination or cervical screening.
Diagnosing a pelvic organ prolapse
Your healthcare provider will ask you about any symptoms you have and how they affect your daily life. They will usually need to do a pelvic exam. They will ask for your consent to do this and you can have a support person with you if needed.
They may also look at your cervix using an instrument called a speculum, which they put into your vagina.
Treating a pelvic organ prolapse
The way a prolapse is treated depends on what type you have and how much it is affecting you.
Lifestyle changes
Your healthcare provider may recommend changes to your lifestyle such as:
You should avoid heavy lifting and getting constipated.
Pelvic floor exercises
You can try exercises to strengthen your pelvic floor muscles. Physiotherapists can help you with these.
Pelvic floor exercises for women
Medicines
If you have a pelvic organ prolapse and have been through menopause, your healthcare provider might prescribe vaginal estrogen cream.
Pessaries
If you try lifestyle changes and still have problems, your healthcare provider may suggest you try a vaginal pessary. This is a small silicone or plastic removable device. It fits into your vagina and adds support to the walls of your vagina. If the pessary is not successful, you may be referred to a women's pelvic health physiotherapist to try a different type of pessary.
Non-surgical treatment for a prolapse
Surgery
If none of these approaches work and your symptoms are really effecting your quality of life, you may be referred to a hospital specialist. They will consider whether surgery may help.
Preventing a pelvic organ prolapse
It is not always possible to prevent a pelvic organ prolapse. But there are things you can do to reduce your risk, including:
- Do pelvic floor exercises every day — strong pelvic floor muscles provide stronger support for your organs.
- Maintain or aim for a healthy weight.
- Avoid constipation — keep physically active, choose foods high in fibre and drink plenty of fluids.
- Protect your pelvic floor when you lift — bend at your knees and keep your back straight when lifting heavy objects.
- Do not smoke — it can lead to chronic coughing, which can put pressure on your pelvic floor muscles.